Egg donation
What is egg donation?
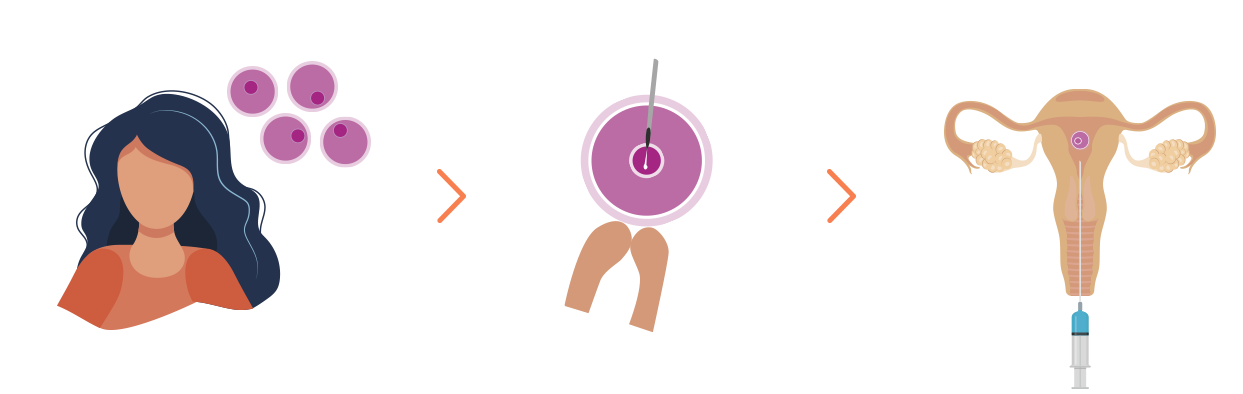
Egg donation is when a woman (donor) gives her eggs to another woman (recipient) to allow the recipient to conceive and have a baby.
The donor’s eggs are fertilised with the recipient couple’s semen or, if necessary, with donor semen.
The eggs obtained are transferred to the recipient’s uterus for them to implant and result in pregnancy. The embryo recipient will carry the child and give birth and will be the legal mother of the new-born.
Egg donation Treatment; There will be no mention of the egg donation in any legal documents (family book, birth certificate, etc.).
When is Egg Donation indicated?
We recommend this treatment in cases such as, various unsuccessful In-vitro fertilisation treatments, menopause, ovaries that have stopped working prematurely (early ovarian failure) or the lack of ovaries.
It is also indicated to couples who could transmit a genetic pathology to their future child.
Egg donation pregnancy rate
Clinical pregnancy rate detecting a heart beat
%
First transfer
%
Accumulated rate
Procedure of egg donation
- 1. Donor selection.
- 2. Preparation of the recipient mother.
- 3. Ovarian stimulation
- 4. Ovarian puncture
- 5. Fertilisation in laboratory
- 6. Embryo transfer
- 7. Vitrification of unused embryos
- 8. Confirmation of pregnancy
- 9. Ultrasound scan
In Spain egg donation is totally legal, it is established by law as anonymous and voluntary.
At Clinica Fertia, donors undergo extensive medical controls, which include interviews, medical tests (examination, analyses, ultrasound scans, etc.) in order to check their physical health and guarantee they are not carriers of any type of hereditary disease.
Clinica Fertia has a large number of donors, which makes it possible to find donors with physical characteristics similar to those of the recipient. Waiting time is normally approximately two to three weeks, although it can be longer, particularly when the recipients are non-Caucasian.
Donors are exclusive, that is, each donor donates her eggs for a single recipient. The average number of oocytes obtained is between 8 and 10, a high number of oocytes results in poorer quality given that many of them carry genetic anomalies (aneuploidy).
Following selection of the optimum donor, the donor and the recipient’s cycles are synchronised. We ensure that the receptor’s ovarian activity ceases, for which contraceptives are usually used or administration of a single dose of GNRHs, except in women who have entered the menopause, in which case it is not necessary.
The next step, an oestrogen substitute regimen is administered either orally or via transdermal patches, to ensure the adequate preparation of the endometrium, where the embryos will be deposited.
During this process one or two ultrasound scans will be done to check that the endometrium has reached the desired thickness. This stage usually takes around two weeks.
In a natural cycle the woman only produces one egg. The same hormones that control the natural cycle are administered to the donor in very high doses, in order to obtain an average of 8-10 eggs. This process lasts around 10-12 days. Throughout this entire stage ultrasound scans are carried out to monitor the number and size of the growing follicle. At the same time it is checked that the receptor’s endometrium is developing properly.
Once the follicles have grown sufficiently a final dose of hormones is given to complete egg maturation and their harvesting at 36 hours is programmed..

This consists in aspiration of the eggs, guided by a transvaginal ultrasound scan, following which the receptor is informed on the number of oocytes obtained, as well as the instructions to initiate a treatment with progesterone.

Once the eggs have been harvested, these are inseminated with the semen of the woman’s partner, previously prepared in the laboratory. Spermatozoid collection may be carried out using a technique called MACS, immunomagnetic selection of the spermatozoids with the greatest capacity to fertilise the egg, or using conventional capture methods.
Fertilisation is carried out using a technique called intracytoplasmic sperm injection (ICSI), which consists in inserting a single previously selected live spermatozoid inside the egg, thanks to which it is possible to carry out fertilisation in the event of poor spermatozoid quality.
When necessary donor semen may be used.
Alternatively, a TESE technique may be used, which consists in ICSI using spermatozoids obtained via testicular biopsy, in cases of obstructive azoospermia, or when ejaculation causes serious damage to the spermatozoids.
The number of oocytes fertilised is checked the following day; the biologist informs daily on their development until transfer day.

This consists in depositing the embryos inside the uterine cavity through a fine cannula that carries the embryos, which is inserted through a speculum previously placed in the vagina. The procedure, which is controlled with the aid of an ultrasound scan, is quick and painless.
Transfer is carried out between two to six days following the puncture, although it is usually after three days have elapsed. A recommendation is usually given on the number of embryos to be transferred, but the final decision is always the couple’s.
After transfer we recommend relative bed rest during the rest of the day and the following one, after which the women can return to her normal activities. Our only recommendation is that the woman avoids any intense or sports activities and abstains from sexual relations during the following two weeks. Travelling is not a problem.
If the option to freeze the remaining embryos of good quality is chosen, these are preserved in liquid nitrogen -technique that is called vitrification- so that they may be used in subsequent cycles, if transfer of fresh embryos fails, in the event of miscarriage or when couples wish to have another baby after having their first, without the need to carry out the entire process again.
A BHCG blood test can be carried out 12 days after embryo transfer.
Alternatively, a urine test can be carried out 14 days after the transfer.
The medication prescribed on the day of the transfer should be continued until pregnancy has been confirmed.

Once 15 days have elapsed from the BHCG test, a scan is done to confirm the existence of a gestational sac and monitoring at the centre will be maintained until heartbeat is found. It is recommended that the hormone substitute treatment is maintained at least until the tenth week of pregnancy.
Frequently asked questions about reproduction treatments
If you would like more information about our treatments, we are always available to help and answer any of your questions.
How long do I have to wait to start treatment?
How many attempts can I make?
In the case of artificial insemination, here at the clinic we recommend a maximum of four attempts, since 90% of pregnancies occur in the first four cycles.
Regarding In-vitro fertilisation or microinjection, our clinic never makes more than four attempts using these techniques.
In the case of egg donation, it is more difficult to establish a limit, this will normally be determined by psychological and also economic factors.
Can you use these techniques when you have already entered menopause?
In these cases, the reception of eggs from a donor must be used.
What are the biggest concerns of egg or sperm recipient couples?
Another factor that concerns a couple is the health of the donors and the physical resemblance to them.
In our centre, both in the case of sperm donors and egg donors, our goal is to seek that the physical resemblance is as similar as possible to the parents.
Are these treatments expensive?
Clínica Fertia is a pioneer in maintaining an honest and transparent policy. Since 2002 we have published the information of the cost of our treatments on our website.
Treatment Price
Patients who come to Fertia are informed from the very first moment with complete transparency about the cost of our treatments.
If you have any questions, consult our team.
Egg donation |
|
Treatment includes: First Visit Donor selection and preparation Medication, analysis and genetic markers Stimulation and ultrasound controls Oocyte retrieval and fertilisation Embryo culture and assisted hatching Endometrial preparation of recipient Embryo transfer to recipient Ultrasound for the recipient |
€6,700 |